
How can managers support employees' mental health?
Louise Fernand • Apr 8, 2024
This blog explores the impact stress can have on teams and offers suggestions for managers to best support employees' mental health.

Louise Fernand • Apr 8, 2024
This blog explores the impact stress can have on teams and offers suggestions for managers to best support employees' mental health.

Louise Fernand • Apr 2, 2024
If you're concerned about your employees becoming stressed at work, have a look at these six behavioural signs of workplace stress.
Alice Squires • Mar 26, 2024
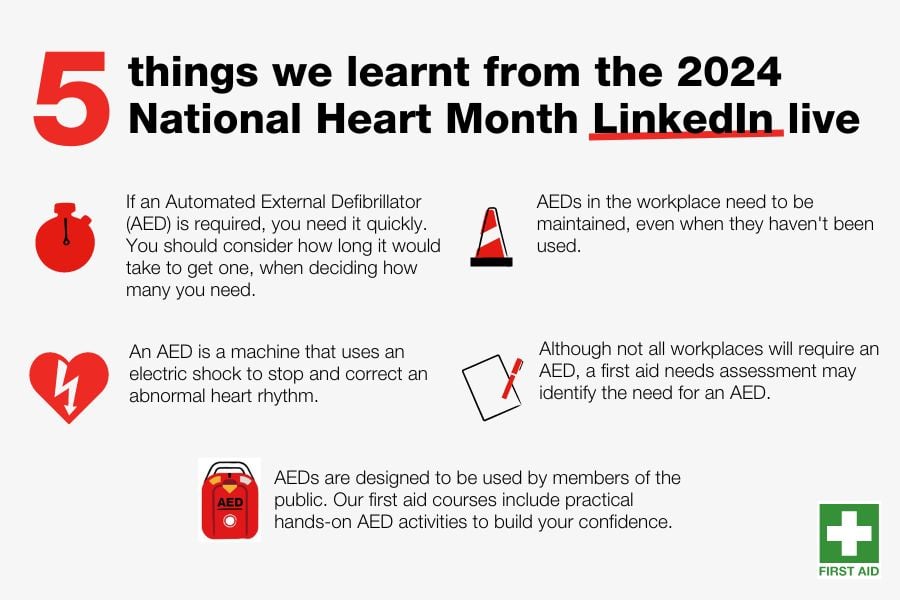
Red Cross Training hosted a LinkedIn live featuring automated external defibrillators (AEDs). Catch up on the session, featuring a live AED demonstration.

Alice Squires • Mar 26, 2024
In support of Purple Day, Alice Squires at British Red Cross Training and Simon Privett, at Epilepsy Action, answer some common questions around epilepsy.

Louise Fernand • Mar 26, 2024
The six online courses equip employees, managers and business owners with proactive and preventative mental health at work training.

Alice Squires • Feb 8, 2024
Investing in quality first aid training makes sure the first aiders in your workplace have the confidence and skills to use CPR and AEDs in an emergency.

Alice Squires • Feb 1, 2024
Learn the benefits of health and safety measures such as defibrillators (AEDs) in the workplace, and how these contribute to building a culture of safety.